What’s new this flu season?
A few things are new this season:
- Flu vaccines are updated to better match viruses expected to be circulating in the United States.
- The A(H1N1)pdm09 vaccine component was updated from an A/Michigan/45/2015 (H1N1)pdm09-like virus to an A/Brisbane/02/2018 (H1N1)pdm09-like virus.
- The A(H3N2) vaccine component was updated from an A/Singapore/INFIMH-16-0019/2016 A(H3N2)-like virus to an A/Kansas/14/2017 (H3N2)-like virus.
- Both B/Victoria and B/Yamagata virus components from the 2018-2019 flu vaccine remain the same for the 2019-2020 flu vaccine.
- All regular-dose flu shots will be quadrivalent. (No trivalent regular-dose flu shots will be available this season.)
- All recombinant vaccine will be quadrivalent. (No trivalent recombinant vaccine will be available this season.)
- All four of the vaccine viruses used to produce cell-grown flu vaccine will have been grown in cells, not eggs.
- In January 2019, the U.S. Food and Drug Administration (FDA) approved a change in dose volume for Fluzone Quadrivalent, a quadrivalent inactivated influenza vaccine.
- The change in dose volume affects children 6 through 35 months of age.
- Previously, children in this age group were recommended to receive 0.25 milliliters of this vaccine per dose.
- Children 6 through 35 months of age may now receive either 0.25 milliliters or 0.5 milliliters per dose.
- There is no preference for one or the other dose volume for this age group. All persons 36 months (or 3 years) of age and older should receive 0.5 milliliters per dose.
- In October 2018, FDA approved an expanded age indication for Afluria Quadrivalent, a quadrivalent inactivated influenza vaccine. Afluria Quadrivalent is now licensed for children 6 months of age and older. Children 6 months through 35 months of age should receive 0.25 milliliters for each dose. All persons 36 months (or 3 years) of age and older should receive 0.5 milliliters for each dose.
- Baloxavir marboxil (trade name Xofluza®) is a new flu single-dose antiviral drug approved October 24, 2018 by FDA. Baloxavir is currently approved by the FDA for treatment of acute uncomplicated influenza within 2 days of illness onset in people 12 years and older who are otherwise healthy, or at high risk of developing influenza-related complications. More information is available here: Influenza Antiviral Drug Baloxavir Marboxil.
- For the 2019-2020 flu season, CDC is offering additional guidance on timing of flu vaccination for both adults and children.
- Like last season, CDC and ACIP recommend that vaccination be offered by the end of October.
- For this season, CDC and ACIP provided additional information on what might be considered vaccinating too early. “Vaccinating early – for example, in July or August –may lead to reduced protection against influenza later in the season, particularly among older adults.”
- Children 6 months through 8 years of age who need 2 doses should receive their first dose as soon as possible after vaccine becomes available to allow the second dose (which must be administered at least 4 weeks later) to be received by the end of October.
For more information on 2019-2020 influenza vaccine recommendations: Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices — United States, 2019–20 Influenza Season
What flu vaccines are recommended this season?
For the 2019-2020 flu season, providers may choose to administer any licensed, age-appropriate flu vaccine (IIV, RIV4, or LAIV4).
Options this season include:
There is a table showing all flu vaccines that are FDA-approved for use in the United States during the 2019-2020 season.
What viruses will the 2019-2020 flu vaccines protect against?
There are many different flu viruses and they are constantly changing. The composition of U.S. flu vaccines is reviewed annually and updated as needed to match circulating flu viruses. Flu vaccines protect against the three or four viruses (depending on the vaccine) that research suggests will be most common. For 2019-2020, trivalent (three-component) vaccines are recommended to contain:
- A/Brisbane/02/2018 (H1N1)pdm09-like virus (updated)
- A/Kansas/14/2017 (H3N2)-like virus (updated)
- B/Colorado/06/2017-like (Victoria lineage) virus
Quadrivalent (four-component) vaccines, which protect against a second lineage of B viruses, are recommended to contain:
- the three recommended viruses above, plus B/Phuket/3073/2013-like (Yamagata lineage) virus.
FDA’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) chooses the flu vaccine viruses for the United States. For 2019-2020 vaccines, they selected the H1N1 and B components on March 6, 2019.external icon Selection of the H3N2 component was delayed until March 22, 2019.
Because the timing of the onset, peak and end of flu seasons varies from year to year and cannot be predicted, it is difficult to say when is the best time to be vaccinated for any one season. In trying to balance the need to get many people vaccinated before flu activity begins with concerns about potential waning of vaccine-induced immunity during the flu season, CDC and ACIP recommend that vaccination be offered by the end of October.
Children 6 months through 8 years of age who need 2 doses should receive their first dose as soon as possible after the vaccine becomes available to allow the second dose (which must be administered at least 4 weeks later) to be received by the end of October.
For people who need only one dose for the season, vaccinating early – for example, in July or August –may lead to reduced protection against flu later in the season, particularly among older adults. While vaccination should optimally occur before the onset of flu activity in the community, providers should continue to offer and encourage vaccination as long as flu viruses are circulating and unexpired vaccine is available. To avoid missed opportunities for vaccination, vaccination can be offered during routine health care visits and hospitalizations.
Can I get a flu vaccine if I am allergic to eggs?
The recommendations for people with egg allergies are unchanged and as follows:
- Persons who are able to eat lightly cooked egg (e.g., scrambled egg) without reaction are unlikely to be egg-allergic.
- Persons who have experienced only hives after exposure to egg should receive any licensed, recommended, age-appropriate flu vaccine (i.e., IIV, RIV4, or LAIV4).
- Persons reporting symptoms other than hives after exposure to egg (such as angioedema, respiratory distress, lightheadedness, or recurrent emesis; or who required epinephrine or another emergency medical intervention) may also receive any licensed and recommended flu vaccine that is otherwise appropriate.
- Additionally, for these persons, vaccine should be administered in an inpatient or outpatient medical setting and supervised by a health care provider who is able to recognize and manage severe allergic reactions.
- A previous severe allergic reaction to flu vaccine, regardless of the component suspected of causing the reaction, is a contraindication to future receipt of the vaccine.
Implications of Cell-Based Vaccines
Why is it significant that cell-grown vaccine viruses are used to produce one flu vaccine?
Cell-grown vaccine viruses do not have changes that may be present in egg-grown reference viruses, so they should be more similar to circulating “wild-type” viruses. Vaccine effectiveness depends in part on the match between the vaccine virus and circulating flu viruses.
Is flu vaccine made using a cell-grown vaccine virus and cell-based technology more effective than vaccine made using an egg-grown vaccine virus and egg-based technology?
While the use of cell-grown vaccine viruses and cell-based technology may offer the potential for better protection over traditional, egg-based flu vaccines because they result in vaccine viruses that are more similar to flu viruses in circulation, there are no vaccine effectiveness data to support this. There is no preferential recommendation for one flu vaccine over another.
Flu Activity
What sort of flu season is expected this year?
Influenza is unpredictable. While flu spreads every year, the timing, severity, and length of the season varies from one season to another.
Will new flu viruses circulate this season?
Flu viruses are constantly changing so it’s not unusual for new flu viruses to appear each year. More information about how flu viruses change is available.
Will the United States have a flu epidemic?
The United States experiences annual epidemics of seasonal flu. This time of year is called “flu season.” In the United States, flu viruses are most common during the fall and winter months. Flu activity often begins to increase in October and November. Most of the time flu activity peaks between December and February, and it can last as late as May. CDC monitors certain key flu indicators (for example, outpatient visits of influenza-like illness (ILI), the results of laboratory testing and reports of flu hospitalizations and deaths). When these indicators rise and remain elevated for a number of consecutive weeks, “flu season” is said to have begun. Usually ILI increases first, followed by an increase in flu-associated hospitalizations, which is then followed by increases in flu-associated deaths.
For the most current flu surveillance information: Weekly U.S. Influenza Surveillance Report.
When will flu activity begin and when will it peak?
The timing of flu is unpredictable and can vary in different parts of the country and from season to season. Seasonal flu viruses can be detected year-round; however, seasonal flu activity often begins as early as October and November and can continue to occur as late as May. Flu activity most commonly peaks in the United States between December and February.
Protective Actions
What should I do to protect myself from flu this season?
CDC recommends a yearly flu vaccine for everyone 6 months of age and older as the first and most important step in protecting against this potentially serious disease.
In addition to getting a seasonal flu vaccine, you can take everyday preventive actions like staying away from sick people and washing your hands to reduce the spread of germs. If you are sick with flu, stay home from work or school to prevent spreading flu to others. In addition, there are prescription medications called antiviral drugs that can be used to treat flu illness.
What should I do to protect my loved ones from flu this season?
Encourage your loved ones to get vaccinated. Vaccination is especially important for people at high risk of developing flu complications, and their close contacts. Also, if you have a loved one who is at high risk of developing flu complications and they get flu symptoms, encourage them to seek medical attention for possible treatment with a flu antiviral drug. These drugs work best if given within 48 hours of when symptoms start. CDC recommends that people who are at high risk of developing serious flu complications and who get flu symptoms during flu season be treated with flu antiviral drugs as quickly as possible without waiting for confirmatory testing. People who are not at high risk of developing serious flu complications may also be treated with flu antiviral drugs, especially if treatment can begin within 48 hours.
Do some children require two doses of flu vaccine?
As in previous seasons, some children 6 months through 8 years of age will need 2 doses of flu vaccine this season. Children in this age group who have not previously received two or more total doses of any trivalent or quadrivalent flu vaccine (including the nasal spray vaccine) before July 1, 2019, or whose vaccination history is not known, need two doses of 2019-2020 flu vaccine administered at least 4 weeks apart.
For 8-year-olds who need two doses, the second dose is recommended even if the child turns 9 years of age between receipt of dose 1 and dose 2. Children in this age group who have received two or more total doses of trivalent or quadrivalent flu vaccine before July 1, 2019 need only one dose for this season.
What can I do to protect children who are too young to get vaccinated?
Children younger than 6 months old are at high risk of serious flu complications, but are too young to get a flu vaccine. Because of this, safeguarding them from flu is especially important. If you live with or care for an infant younger than 6 months old, you should get a flu vaccine to help protect them from flu. Advice for Caregivers of Young Children is available for more information. Everyone else who is around the baby also should be vaccinated. Also, studies have shown that flu vaccination of the mother during pregnancy can protect the baby after birth from flu infection for several months.
In addition to getting vaccinated, you and your loved ones can take everyday preventive actions like staying away from sick people and washing your hands to reduce the spread of germs. If you are sick with flu, stay home from work or school to prevent spreading flu to others.
Vaccine and Vaccination
How much flu vaccine will be available this season?
Flu vaccine is produced by private manufacturers, so supply depends on manufacturers. For the 2019-2020 season, manufacturers have projected they will provide as many as 162 million to 169 million doses of flu vaccine, which is similar to projected supply for last season. Flu vaccine supply updates will be provided as they become available at Seasonal Influenza Vaccine & Total Doses Distributed.
Are any of the available flu vaccines recommended over the others?
For the 2019-2020 flu season, ACIP recommends annual flu vaccination for everyone 6 months and older with any licensed, age-appropriate flu vaccine (IIV, RIV4, or LAIV4) with no preference expressed for any one vaccine over another.
There are many vaccine options to choose from; the most important thing is for all people 6 months and older to get a flu vaccine every year. If you have questions about which vaccine is best for you, talk to your doctor or other health care professional.
Why is the nasal spray being recommended as an option this year when it has been shown to not be effective in past flu seasons?
Flu vaccine effectiveness (VE) can vary from year to year, among different age and risk groups, by vaccine type, and even by virus type and subtype. While data from 2010-2011 through 2016-2017 indicated that nasal spray vaccine lacked effectiveness among 2 through 17-year-olds against H1N1 viruses in the U.S., nasal spray vaccine was effective against influenza B viruses, and was similarly effective against H3N2 viruses as inactivated influenza vaccines. Since the 2018-2019 season, the manufacturer of nasal spray vaccine has used a new H1N1 vaccine virus in production. Some data suggest this will result in improved effectiveness of against H1N1. However, no published effectiveness estimates for this vaccine component against H1N1 viruses are available. ACIP and CDC voted to resume the recommendation for the use of nasal spray vaccines based on evidence suggesting that the new H1N1 component will result in improved effectiveness of the vaccine against these viruses. There is no expressed preference for any flu shot or the nasal spray vaccine.
Where can I get a flu vaccine?
Flu vaccines are offered by many doctor’s offices, clinics, health departments, pharmacies and college health centers, as well as by many employers, and even by some schools.
Even if you don’t have a regular doctor or nurse, you can get a flu vaccine somewhere else, like a health department, pharmacy, urgent care clinic, and often your school, college health center, or work.
The HealthMap Vaccine Finderexternal icon helps you to locate where you can get a flu vaccine.
What is flu vaccination using a jet injector?
FDA has approved one flu vaccine (Afluria Quadrivalent) for administration by a jet injector device (the PharmaJet Stratis 0.5ml Needle-free Jet Injector) for people 18 through 64 years of age. These are the only two flu vaccines approved for administration by jet injector. People aged 18 through 64 years may receive this vaccine either by jet injector or needle. A jet injector is a medical device used for vaccination that uses a high-pressure, narrow stream of fluid to penetrate the skin instead of a hypodermic needle. More information about Flu Vaccination by Jet Injector is available.
What is adjuvanted flu vaccine?
The FDA licensed a seasonal flu vaccine containing adjuvant for adults 65 years of age and older. An adjuvant is an ingredient added to a vaccine to create a stronger immune response to vaccination. FLUAD™Cdc-pdfpdf icon[155 KB, 13 pages]external icon was licensed in November 2015 and will be available during the 2019-2020 flu season. It includes the MF59 adjuvant, an oil-in-water emulsion containing squalene oil. FLUAD™ is the first adjuvanted seasonal flu vaccine marketed in the United States.
Can I get vaccinated and still get flu?
Yes. It’s possible to get sick with flu even if you have been vaccinated (although you won’t know for sure unless you get a flu test). This is possible for the following reasons:
- You may be exposed to a flu virus shortly before getting vaccinated or during the period that it takes the body to gain protection after getting vaccinated. This exposure may result in you becoming ill with flu before the vaccine begins to protect you. (Antibodies that provide protection develop in the body about 2 weeks after vaccination.)
- You may be exposed to a flu virus that is not included in the seasonal flu vaccine. There are many different flu viruses that circulate every year. A flu vaccine is made to protect against the three or four flu viruses that research suggests will be most common.
- Flu vaccine varies in how well it works, and unfortunately, some people can become infected with a flu virus that a flu vaccine is designed to protect against, despite getting vaccinated. Protection provided by flu vaccination can vary widely, based in part on health and age factors of the person getting vaccinated. It also can vary based on the match between the vaccine viruses used to produce vaccine and circulating viruses that season. In general, a flu vaccine works best among healthy younger adults and older children. Some older people and people with certain chronic illnesses may develop less immunity after vaccination. Flu vaccination is not a perfect product, but it is the best way to protect against flu infection.
- Even if you do get the flu after being vaccinated, some studies have shown that a flu vaccine can reduce the severity of your illness.
- A 2017 study showed that flu vaccination reduced deaths, intensive care unit (ICU) admissions, ICU length of stay, and overall duration of hospitalization among hospitalized flu patients.
- A 2018 studyexternal icon showed that among adults hospitalized with flu, vaccinated patients were 59 percent less likely to be admitted to the ICU than those who had not been vaccinated. Among adults in the ICU with flu, vaccinated patients on average spent 4 fewer days in the hospital than those who were not vaccinated.
Flu Vaccine Effectiveness
How effective will flu vaccines be this season?
It’s not possible to say in advance exactly how well the flu vaccine will work this season. How well it works can vary by season, virus type/subtype, the kind of vaccine, and age and other host factors of the people being vaccinated. At least two factors play an important role in determining the likelihood that flu vaccines will protect a person from flu illness: 1) characteristics of the person being vaccinated (such as their age and health), and 2) the similarity or “match” between the flu viruses in the vaccine and those spreading in the community.
During years when the viruses in the flu vaccine and circulating flu viruses are well matched, it’s possible to measure substantial benefits from flu vaccination in terms of preventing flu illness. However, even during years when the vaccine match is good, the benefits of flu vaccination will vary across the population, depending on host factors like the health and age of the person being vaccinated and even potentially which flu vaccine was used.
Recent studies by CDC researchers and other researchers suggest that flu vaccination usually reduces the risk of influenza illness by 40% to 60% among the overall population when the vaccine viruses are like the ones spreading in the community.
For more information about vaccine effectiveness, click here.
Will this season’s flu vaccine be a good match for circulating viruses?
It’s not possible to predict with certainty if a flu vaccine will be a good match for circulating flu viruses. A flu vaccine is made to protect against the flu viruses that research and surveillance indicate will likely be most common during the season. However, scientists must pick which flu viruses to include in a flu vaccine many months in advance in order for flu vaccines to be produced and delivered on time. Also flu viruses change constantly (called “drift”). They can change from one season to the next or they can even change within the course of one flu season. Another factor that can impact vaccine effectiveness, especially against influenza A(H3N2) viruses, are changes that can occur in vaccine viruses as they are grown in eggs, which is the production method for most current flu vaccines. Because of these factors, there is always the possibility of a less than optimal match between circulating flu viruses and the viruses in a flu vaccine.
Over the course of flu season, CDC studies samples of circulating flu viruses to evaluate how close a match there is between viruses used to make the flu vaccine and circulating flu viruses.
One of the ways that helps CDC evaluate the match between flu vaccine viruses and circulating flu viruses is with a lab process called ‘genetic and antigenic characterization’. Results of genetic and antigenic characterization testing are published weekly in CDC’s FluView.
Can a flu vaccine provide protection even if the flu vaccine is not a “good” match?
Yes, antibodies made in response to vaccination with one flu virus sometimes can provide protection against different but related flu viruses. A less than ideal match may result in reduced vaccine effectiveness against the flu virus that is different from what is in the flu vaccine, but it might still provide some protection against flu illness.
In addition, it’s important to remember that a flu vaccine contains three or four flu viruses (depending on the type of vaccine you receive) so that even when there is a less than ideal match or lower effectiveness against one virus, a flu vaccine may protect against the other flu viruses.
For these reasons, even during seasons when there is a less than ideal match, CDC continues to recommend flu vaccination for everyone 6 months and older. Vaccination is particularly important for people at high risk for serious flu complications), and their close contacts.
If You Get Sick
What happens in the body when someone has flu?
Flu viruses usually infect the respiratory tract (i.e., the airways of the nose, throat and lungs). As the infection progresses, the body’s immune system responds to fight the virus. This results in inflammation that can trigger respiratory symptoms such as cough and sore throat. The immune system response also can trigger fever and cause muscle or body aches. When infected people cough, sneeze, or talk, they can spread flu viruses in respiratory droplets to people who are nearby. People might also get flu by touching a contaminated surface or object that has flu virus on it and then touching their own mouth or nose.
Most people who become sick will recover in a few days to less than two weeks, but some people may become more severely ill. Following flu infection, moderate complications such as secondary ear and sinus infections can occur. Pneumonia is a serious flu complication that can result from either flu virus infection alone or from co-infection of flu virus and bacteria. Other possible serious complications triggered by flu can include inflammation of the heart (myocarditis), brain (encephalitis) or muscle (myositis, rhabdomyolysis) tissues, and multi-organ failure (for example, respiratory and kidney failure). Severe complications can happen to anyone, but may be more likely to happen to people who have certain chronic medical conditions, or in elderly persons.
What should I do if I get sick with flu?
Most people with flu have mild illness and do not need medical care or antiviral drugs. If you get sick with flu symptoms, in most cases, you should stay home and avoid contact with other people except to get medical care.
If, however, you have symptoms of flu and are at high risk of flu complications, or are very sick or concerned about your illness, contact your health care provider. There are drugs your doctor may prescribe for treating flu called antivirals. These drugs can make you better faster and may also prevent serious complications.
Antiviral drugs are prescription drugs that can be used to treat flu illness. People at high risk of serious flu complications recommended for prompt antiviral treatment include children younger than 2 years of age (although all children younger than 5 years are considered at higher risk for complications from flu, the highest risk is for those younger than 2 years of age), adults 65 years of age and older, pregnant women, people with certain long-term medical conditions, and residents of nursing homes and other long-term care facilities). Antiviral treatment as early as possible is also recommended for people who are very sick with flu (such as those with complicated, progressive illness or people hospitalized because of flu). Other people can be treated with antivirals at their health care professional’s discretion. Treating high risk people or people who are very sick with flu with antiviral drugs is very important. Studies show that prompt treatment with antiviral drugs can prevent serious flu complications. Prompt treatment can mean the difference between having a milder illness versus very serious illness that could result in a hospital stay.
Treatment with antivirals works best when begun within 48 hours of getting sick. However, treatment can still be beneficial when given later in the course of illness. Antiviral drugs are effective across all age and risk groups. Studies show that antiviral drugs are under-prescribed for people who are at high risk of complications who get flu. Four FDA-approved antiviral medications are recommended for use during the 2019-2020 flu season: oseltamivir (available in generic versions and under the trade name Tamiflu®), zanamivir (Relenza®), peramivir (Rapivab®), and baloxavir marboxil (Xofluza®). More information about antiviral drugs can be found at Treatment – Antiviral Drugs. This guidance is consistent with the 2019-2020 flu season recommendationsexternal icon published by the Infectious Diseases Society of America (IDSA) on December 19, 2018, in Clinical Infectious Diseases.
“The Flu: What To Do If You Get Sick”
What is baloxavir marboxil?
Baloxavir marboxil (trade name Xofluza®) is a flu single-dose antiviral drug approved October 24, 2018 by the FDA. Baloxavir is approved for the treatment of acute uncomplicated flu in people 12 years and older who have had flu symptoms for less than 48 hours. In clinical randomized trials, baloxavir was similar to oseltamivir, a currently recommended flu antiviral drug, in alleviating flu symptoms.
More information regarding baloxavir is available: Influenza Antiviral Drug Baloxavir Marboxil.
Surveillance
How does CDC track flu activity?
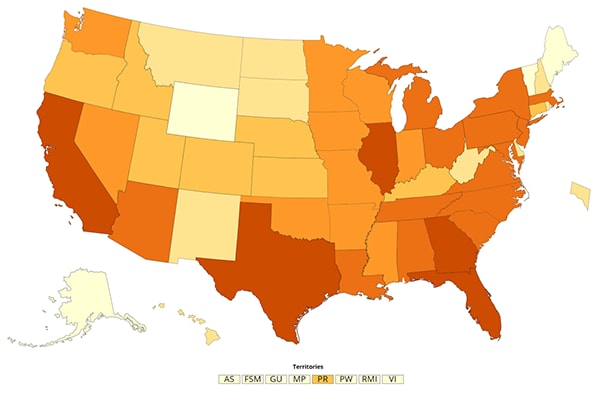
The Epidemiology and Prevention Branch in the Influenza Division at CDC collects, compiles and analyzes information on flu activity year round in the United States and produces FluView, a weekly flu surveillance report, and FluView Interactive, which allows for more in-depth exploration of flu surveillance data. The U.S. flu surveillance system is a collaborative effort between CDC and its many partners in state, local, and territorial health departments, public health and clinical laboratories, vital statistics offices, healthcare providers, clinics, and emergency departments. Information in five categories is collected from eight different data sources that allow CDC to:
- Find out when and where flu activity is occurring
- Track flu-related illness
- Determine what flu viruses are circulating
- Detect changes in flu viruses
- Measure the impact flu is having on hospitalizations and deaths in the United States
For more information, visit “Overview of Influenza Surveillance in the United States”.
What will CDC do to monitor flu vaccine effectiveness for the 2019-2020 season?
CDC collaborates with partners each season to assess how well the seasonal flu vaccines are working. During the 2019-2020 season, CDC is planning multiple studies on the effectiveness of flu vaccines. Researchers conduct these studies each year to measure how well flu vaccines work in order to continually assess and confirm their value as a public health measure.
Part of the need for this continued assessment is that flu viruses that circulate each year tend to change and evolve, and so the components of the flu vaccine are changed relatively frequently to protect against these new circulating viruses. A summary of CDC’s latest vaccine effectiveness estimates is available at Seasonal Influenza Vaccine Effectiveness, 2005-2018.
What is CDC doing to monitor antiviral resistance in the United States during the 2019-2020 season?
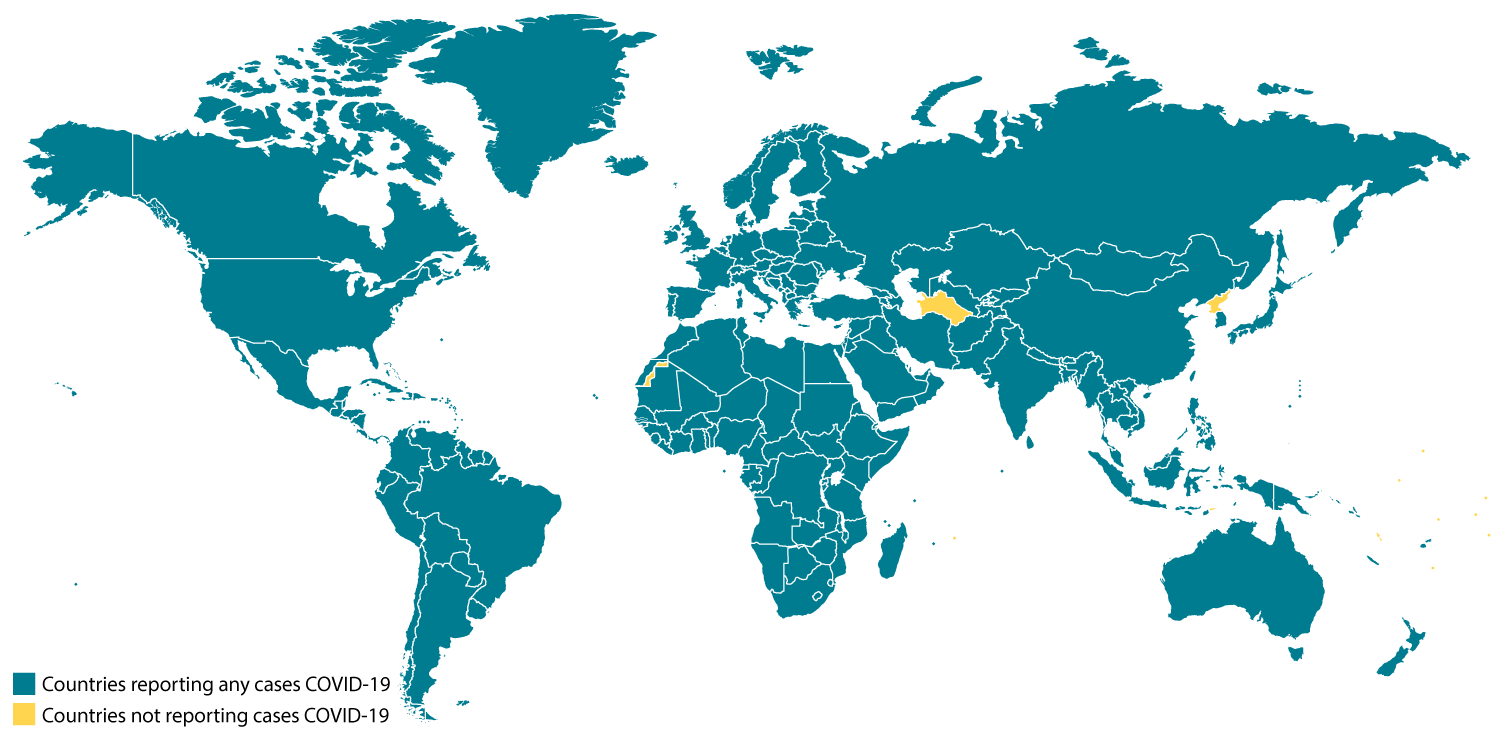
Antiviral resistance means that a virus has changed in such a way that antiviral drugs are less effective or not effective at all in treating or preventing illnesses with that virus. CDC will continue to collect and monitor flu viruses for changes through an established network of domestic and global surveillance systems. CDC also is working with the state public health departments and the World Health Organization to collect additional information on antiviral resistance in the United States and worldwide. The information collected will assist in making informed recommendations regarding use of antiviral drugs to treat flu.
How does CDC estimate the burden of seasonal flu on the United States?
The burden of flu on the United States can vary widely from season to season and is determined by a number of factors including the characteristics of circulating viruses, the timing of the season, population immunity to circulating viruses, how well flu vaccines are working, and how many people have gotten vaccinated. While the impact of flu varies, it places a substantial burden on the health of people in the United States each year.
CDC uses a model to estimate the numbers of flu illnesses, medical visits, and hospitalizations in the United States (as well as the impact of flu vaccination on these numbers). The same model is also extended to estimate flu-related deaths in the United States. This methodology has been used to retroactively calculate flu burden, including deaths, going back to 2010.
Beginning with the 2018-2019 flu season, CDC began reporting cumulative, in-season estimates of the burden of flu. These Preliminary In-Season Burden Estimates will be provided when activity has been sufficient to generate a stable estimate, and will be updated weekly over the course of the flu season.
How does CDC classify flu season severity?
In 2017, CDC adopted and outlined a new methodology for determining flu season severity. Based on data from past flu seasons, CDC researchers used key flu indicator data to develop intensity thresholds (ITs) to classify the severity of flu seasons.
Based on the intensity thresholds, CDC researchers classified seasonal severity from 2003-2004 through the 2018-2019 flu seasons. Overall, four seasons were classified as low severity, eight as moderate, three as high, and none as very high.
What is flu forecasting?
Flu places a significant disease burden on the U.S. population each year, but the magnitude and timing varies from season to season, making the annual impact difficult to predict at the beginning of each season. Flu forecasting may help predict when the start, peak, and increases in flu activity will occur. Unlike CDC’s traditional influenza surveillance systems, which measure flu activity after it has occurred, flu forecasting offers the possibility to look into the future and better plan ahead, potentially reducing the impact of flu and can potentially be used to prepare for and prevent illness, hospitalization, and death, as well as the economic burden, experienced during a flu epidemic. When forecasts accurately predict flu activity, the ability to more effectively plan for public health responses to seasonal flu epidemics and future influenza pandemics is possible.
Flu forecasting aims to predict the characteristics of influenza seasons before disease activity occurs and is captured by the U.S. influenza surveillance system. Since the 2013-2014 flu season, the Influenza Division at CDC has worked with CDC’s Epidemic Prediction Initiative (EPI) and external researchers to improve the science and usability of flu forecasting by coordinating flu forecasting challenges. Recently, these challenges have been extended to state-level predictions and forecasting hospitalization rates.
During 2018-2019, CDC began summarizing and publicly posting flu forecasts. For the 2019-2020 flu season, CDC will continue to display weekly the forecasts received through the EPI.
Learn more about flu forecasting by visiting https://www.cdc.gov/flu/weekly/flusight/index.html.